Application of proteoglycans from fish cartilage for the acceleration of burn wound healing
Abstract
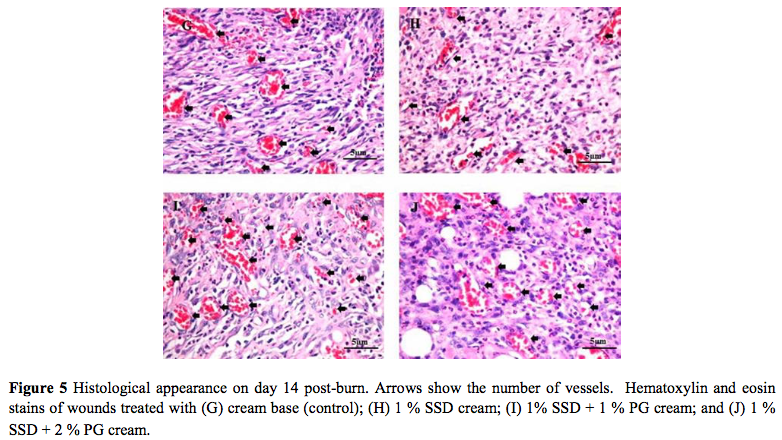
Cartilage contains a variety of proteoglycans (PGs)that can accelerate wound healing. The aim of this study was to evaluate the efficacy of proteoglycans extracted from fish cartilage for the acceleration of burn wound healing. Second degree burn wounds were induced by placing an electrical hot plate set at 90°C for 10 s on the back of rats. Rats were randomly assigned to receive 1 g of cream base (control), 1% silver sulfadiazine (SSD), 1% PG, 2% PG, a combination of 1% SSD + 1% PG, or a combination of 1% SSD + 2% PG applied to burn wounds immediately after burning and once daily until day 27 post-burn. Wound healing was evaluated on days 3, 7, 14, 21 and 28. Histological analysis was performed on days 7, 14 and 21. The percentage wound healing after treatment with cream containing PG was significantly (p<0.001) higher than that in the control group on day 7 post-burn and thereafter. Histological analysis showed that the combination of 1% SSD + 2% PG had the highest efficacy in increasing re-epithelialization and neovascularization in burn wounds. We conclude that PG extracted from fish cartilage can accelerate and facilitate wound healing in rats. The combination of 1% SSD and 1% or 2% PG has high efficacy in accelerating and facilitating wound healing.
Full Text:
64-69:PDFReferences
M.D. Peck. Epidemiology of burns throughout the World. Part II: intentional burns in adults, Burns. 38: 630-637 (2012).
S. Hettiaratchy and P. Dziewulski. ABC of burns. Introduction, BMJ. 328: 1366-1368 (2004).
A.M. Cameron. Burn wound management: a surgical perspective, Wound Practice &Researc. 18: 35-40 (2010).
S. Hettiaratchy and R. Papini. Initial management of a major burn: II- assessment and resuscitation, BMJ. 329: 101-103 (2004).
B.S. Atiyeh, S.N. Hayek, and S.W. Gunn. New technologies for burn wound closure and healing-review of the literature, Burns. 31: 944-956 (2005).
A.J. Singer and A.B. Dagum. Current management of acute cutaneous wounds, N Engl J Med. 359: 1037-1046 (2008).
B.S. Atiyeh, M. Costagliola, S.N. Hayek, and S.A. Dibo. Effect of silver on burn wound infection control and healing: review of the literature, Burns. 33: 139-148 (2007).
J.F. Fraser, L. Cuttle, M. Kempf, and R.M. Kimble. Cytotoxicity of topical antimicrobial agents used in burn wounds in Australasia, J Surg. 74: 139-142 (2004).
T.E. Hardingham, and A.J. Fosang. Proteoglycans: many forms and many functions, FASEB J. 6: 861-870 (1992).
N. Perrimon, and M. Bernfield. Cellular functions of proteoglycans an overview, Semin Cell Dev Biol. 12: 65-67 (2001).
C.B. Knudson, and W. Knudson. Cartilage proteoglycans, Semin Cell Dev Biol. 12: 69-78 (2001).
B. Neelam, N. Titpawan, and N. Teerapol. In vitro stimulatory effect of grandiflorenic acid isolated from Wedeliatrilobata (L.) leaves on L929 fibroblast cells, TJPS. 37: 117-124 (2013).
D. Aviezer, and A. Yayon. Heparin-dependent binding and autophosphorylation of epidermal growth factor (EGF) receptor by heparin-binding EGF-like growth factor but not by EGF, Proc Natl Acad Sci U S A. 91: 12173-12177 (1994).
G. Raab, and M. Klagsbrun. Heparin-binding EGF-like growth factor,BiochimBiophysActa. 1333: 179-199 (1997).
R.L. Gallo. Proteoglycans and cutaneous vascular defense and repair, J Investig Dermatol Symp Proc. 5: 55-60 (2000).
J. Somboonwong, M. Kankaisre, B. Tantisira, and M.H. Tantisira. Wound healing activities of different extracts of Centellaasiatica in incision and burn wound models: an experimental animal study, BMC Complement Altern Med. 12: 103 (2012).
B.E. Zawacki. The natural history of reversible burn injury, Surg Gynecol Obstet. 139: 867-872 (1974).
S.P. Schallberger, B.J. Stanley, J.G. Hauptman, and B.A. Steficek. Effect of porcine small intestinal submucosa on acute full-thickness wounds in dogs, Vet Surg. 37: 515-524 (2008).
J. Li, J. Chen, and R. Kirsner. Pathophysiology of acute wound healing, Clin Dermatol. 25: 9-18 (2007).
S. Guo, and L.A. Dipietro. Factors affecting wound healing, J Dent Res. 89: 219-229 (2010).
B. Mahdavian Delavary, W.M. Veer, M. Egmond, F.B. Niessen, and R.H. Beelen. Macrophages in skin injury and repair, Immunobiology. 216: 753-762 (2011).
S. Enoch, and D.J. Leaper. Basic science of wound healing. Surgery. 26: 31–37 (2005).
I. Mayers, and D. Johnson. The nonspecific inflammatory response to injury, Can J Anaesth. 45: 871-879 (1998).
G. Broughton 2nd, J.E. Janis, and C.E. Attinger. The basic science of wound healing, Plast Reconstr Surg. 117: 12-34 (2006).
Refbacks
- There are currently no refbacks.

